Genetic Risk of Breast Cancer
It’s not an easy thing to hear when you are diagnosed with breast cancer. It’s challenging physically and emotionally.
People wonder why they got it, especially those who lead healthy lifestyles.
That begs the question: do genetics play a role in breast cancer risk?
1. What is cancer?
Cancer covers a variety of diseases that are characterized by uncontrolled cell growth and spread.
Cell growth and division are controlled precisely in normal circumstances, but sometimes, there are genetic mutations that can disrupt this balance.
This can cause unregulated cell proliferation, likely invading nearby tissues.
2. What is breast cancer?
Breast cancer originates in breast tissues.
This includes:
- lobules or milk-producing glands
- ducts or channels that carry milk to the nipple
- connective tissue
Most common breast cancer types are:
- Ductal Carcinoma: Begins in the ducts.
- Lobular Carcinoma: Starts in the lobules.
This cancer can be invasive. It can spread into surrounding breast tissue or non-invasive (in-situ) that can remain confined to the ducts/lobules where it began.
3. What role do genetics play?
Genes are DNA segments. They provide instructions for making proteins that regulate cell functions; we inherit two copies of each gene – one from each parent.
Mutation in specific genes (proto-oncogenes and tumor suppressor genes) can cause cancer by disrupting the normal regulation of cell growth and survival.
You can inherit these:
- from your parents
- because of DNA replication errors
- because of exposure to carcinogenic substances
4. Genetic Factors
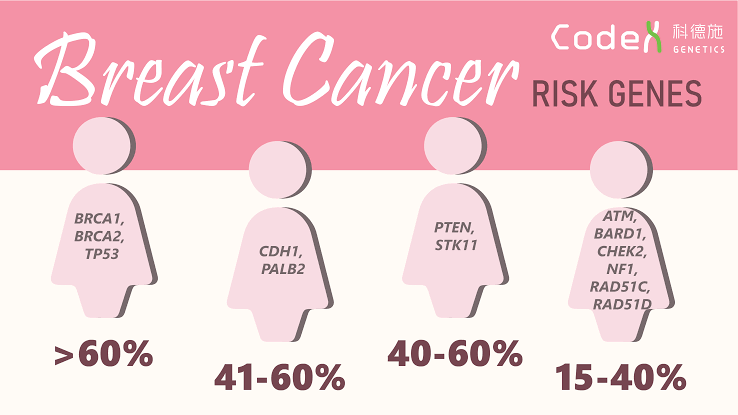
5 – 10% cases are hereditary and genes associated the most with increased breast variant cancer risk are:
- BRCA1
- BRCA2
Those women who have harmful mutations in these genes have up to a 70% chance of developing breast cancer by the time they are 80.
Other genes that are linked to a higher risk of breast cancer are:
- PALB2
- TP53
- PTEN
Mostly, breast cancer results from DNA damage that happens over a lifetime, causing mutation in breast cells.
There are also some lifestyle factors like alcohol consumption, physical inactivity, and obesity that can increase the likelihood of these mutations. Age is not far behind, mostly diagnosed in women over 50.
Diagnosis
Your doctors may recommend different diagnostic tests to check for a lump or other concerning changes to be detected in the breast:
- Mammogram: a low-dose x-ray of the breast to identify abnormalities.
- Ultrasound: uses sound waves to produce an image of the breast tissue to look for a lump and whether it is solid or fluid-filled.
- MRI: magnets and radio waves give a breast image. It’s generally used for high-risk women or to further evaluate suspicious findings.
- Biopsy: a sample is removed from the breast cells or tissues for microscopic examination. The standard method is a core needle biopsy.
If breast cancer is confirmed, additional tests will help to find out about the tumor’s stage and its specific characteristics for further treatment decisions.
Parting Thoughts
This is not to say that all breast cancers are directly inherited or hereditary. But you can’t ignore the fact that genetic factors do influence breast cancer development risk.
Most of these cancers come from changes in breast cells over a period of time. This could be for a number of reasons as we mentioned.
So, if you have a family history of breast cancer, particularly among close relatives like your mother or sister, you should discuss your risk with a doctor. Some people may be advised to get genetic testing.
Even if you’re not considered at risk, as a woman of any age, you should take steps to lower the chances of breast cancer. Look for early detection through healthy lifestyle choices and regular screenings.
For more information, visit Canadian pharmacy